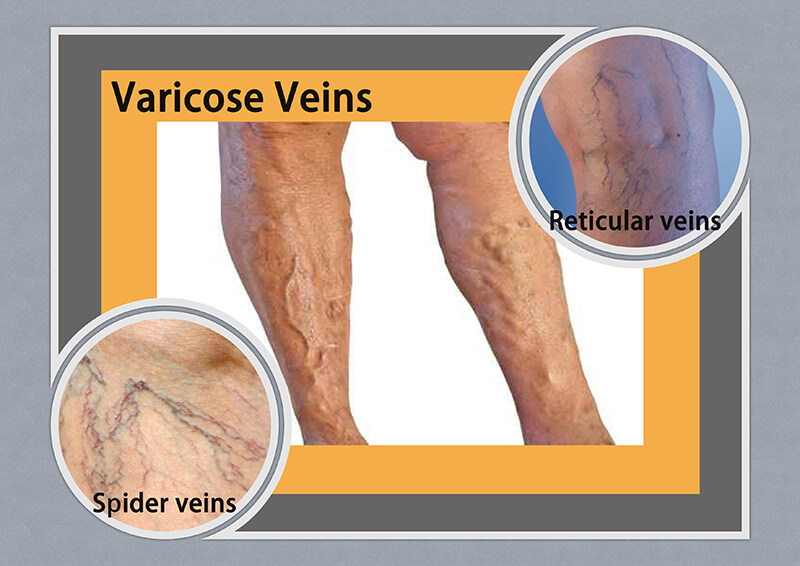
<Pictures of varicose veins>
What is a vein? What is varicose vein?
Veins are an important part of the circulatory system. Veins return blood with low oxygen content, high carbon dioxide content, and high metabolic waste, to the heart. Upper limb, lower limb and body surface veins have valves to keep the blood flow in one direction, i.e. towards the right heart. These venous valves prevent the backflow of blood.
Varicose veins often occur because of degeneration or damage to the venous valves. High venous pressure and venous blood accumulation further damage the veins. With time, wider varicose veins will form.
Venous blood, with low oxygen and increased water pressure, fills the capillaries and affects the microvascular circulation of normal tissues. Normal tissues lack fresh blood supply. The skin and subcutaneous tissues are hypoxic, edematous, inflamed, thickened, and discolored. The tissues will not heal after minor injuries.
Mild varicose veins (Small varicose veins) cause only slight discomfort or poor cosmesis. However, severe varicose veins (Large varicose veins) can seriously affect the normal activities of patients, and can lead to limb disability or limb loss.
Small varicose veins (included spider varicose veins and reticular varicose veins) (usually 1mm-3mm) :
Spider varicose veins refer to spider feet like dilated red or dark red tiny varicose veins. Reticular varicose veins refer to net-like dilated dark red, dark purple, or dark blue tiny varicose veins. Spider veins and reticular veins are similar to regular varicose veins, but are smaller and less bulging. They are more common on women's thighs and legs. Women are several times more likely to develop it than men. Pregnancy and oral contraceptive use may increase the risk.
Large varicose veins (also known as bulging veins or tortuous veins) (usually 4mm -3cm) :
Varicose veins are twisted and dilated veins. Commonly found on the inner thigh, inner calf, back of the calf and outer calf. With the naked eye, you can see blue, purple-red or flesh-colored twisted rope-like raised veins or large worm-like veins below the skin.
Causes
Causes of varicose veins are as follows:
- Genetic
- Aging
- Obesity
- Prolonged standing and sitting jobs, such as nurses, sales person, waiters/waitresses, office workers etc.
- Women affected by estrogen, such as pregnancy, puberty, menopause, or use of oral contraceptive pills etc.
- Abdominal tumors obstructing lower limbs venous return (Rare)
Symptoms
Mild Symptoms (Small Varicose Veins)
- On and off leg heaviness, aching, or burning pain, more obvious after prolonged sitting or standing
- Slight swelling in the lower limbs
- On and off itchy skin over varicose vein
Severe Symptoms (Large Varicose Veins)
- Persistent leg heaviness, aching, or burning pain shortly after sitting or standing
- Leg and ankle severe swelling
- Dark brown or purple skin pigmentation / discoloration
- Dry and itchy skin
- Skin inflammation, thickened skin, and bacterial infection
- Skin thinning and ulcers formation
- Bleeding
- Deep vein thrombosis (rare)
Patient Complaints
Majority of patients complained about several groups of spider veins or tortuous and bulging veins in their lower limbs when they were first seen by doctors. A small portion of patients presented with skin discoloration, skin hardening, inflammation or infection of skin and subcutaneous tissue, lower limb wounds, non-healing venous ulcers, or venous ulcer bleeding.
Diagnosis
Experienced surgeons use clinical assessment (CEAP) to stage varicose veins. The CEAP classification employs a description of the clinical class (C) with objective signs, the etiology (E), the anatomical (A) distribution of reflux and obstruction in the superficial, deep, and perforating veins, and the underlying pathophysiology (P), whether due to reflux or obstruction.
Clinical Assessment Classification
- C0: No visible or palpable signs of venous disease
- C1: Telangiectasia or reticular veins
- C2: Varicose veins
- C3: Edema
- C4a: Pigmentation or eczema
- C4b: Lipodermatosclerosis or atrophie blanche
- C5: Healed venous ulcer
- C6: Active venous ulcer
Etiologic Classification
Etiologic classification is as follows:
- Congenital (i.e., Klippel-Trenaunay syndrome)
- Primary
- Secondary (i.e., post-thrombotic syndrome, trauma)
- No venous cause identified
Anatomic Classification
Anatomic classification is as follows:
- Superficial
- Deep
- Perforator
- No venous location identified
Pathophysiologic Classification
Pathophysiologic classification is as follows:
- Reflux
- Obstruction, thrombosis
- Reflux and obstruction
- No venous pathophysiology identified in advanced stages
Investigation
Before deciding on treatment or surgery, experienced surgeons perform a Color Doppler Ultrasound Scan (CDUS) for the affected lower limbs. CDUS helps to:
- When squeezing and releasing distal veins in the lower extremities, CDUS confirms bidirectional flow of blood. Reverse flow of venous blood is also called backflow, retrograde flow, or reflux.
- Locate the origin and locations of venous backflow
- Confirm deep venous system patency
- Help determine the site for treatment/surgery
- Mark the location of the incision before surgery
Treatments
Varicose Vein Treatments
Varicose vein is a common surgical disease. The majority of patients have mild to moderate disease. Early treatment can prevent the disease from progressing to a severe status or even complications. Treatments can be grouped into non-surgical and surgical treatments.
Non-Surgical Treatments
- Mild varicose veins can be improved by lifestyle changes, medication, and wearing compression stockings to relieve symptoms
- Avoid prolonged sitting or standing
- Frequently elevate legs above heart level to improve venous blood circulation
- Distal to proximal foot, leg, and thigh massage
- Wear compression stockings on calves +/- thighs
- Avoid compression garments on the trunk
- Avoid female hormone treatment
- Medications, e.g., Daflon, Dioflex
Surgical Treatments
After reflux veins are treated, venous blood will return to the heart via normal veins with good functioning valves.
Foam Sclerotherapy / Sclerosant Injection Varicose Vein Therapy
- Suitable for varicose veins <3mm
- Varicose vein foam injection/sclerotherapy injection is suitable for small varicose veins (spider veins or reticular veins). Injectable treatment requires 2 - 3 treatments, once every 6 to 8 weeks.
- Possible side effects include bruising, pigmentation, vein inflammation, and skin necrosis.
- Varicose vein foam injections/sclerotherapy injections do not target the origin of the venous reflux; new spider veins or reticular veins can recur. Please consult your doctor for advice.
Superficial Vein Laser Treatment
- Suitable for varicose veins <3mm
- The laser burns superficial veins and causes minor burns to the skin.
- Superficial vein laser treatment only blocks the superficial veins and does not treat the source of the reflux veins. It may recur after treatment. Please consult your doctor for advice.
Traditional Open Surgery with Multiple Ligations and Stripping
- Surgeons make multiple 2cm to 5cm skin incisions, bring out the varicose veins above the skin, and perform multiple varicose vein ligations and stripping of the long saphenous vein of the thigh.
- These surgeries are very painful and require general or spinal anesthesia in the hospital.
- Patients need to take 1 - 3 weeks of sick leave and can walk normally afterward.
Minimal Invasive Intravascular Mechanical Rotary Irritation and Sclerosant Injection (ClariVein®)
Studies showed that it has a higher recurrence rate than other methods. Please consult your doctor for advice.
Minimal Invasive Endovascular Laser Ablation Treatment (EVLT) or Endovascular Radiofrequency Ablation Treatment (EVRT) of Varicose Veins
- EVLT and EVRT are minimal invasive surgeries specifically designed to treat longer varicose veins.
- Under ultrasound guidance, experienced surgeons make microincisions of 2-5mm near the knee, put a small catheter into the veins (such as the great saphenous vein), and use laser or radiofrequency energy to heat the inside of the veins and cauterize them.
- Veins will be constricted, sealed, and scarred.
- EVLT and EVRT are suitable for more severe varicose veins. The operation takes about thirty to sixty minutes, the wound is small, and the recurrence rate is low.
- These surgeries require injecting a large amount of normal saline diluted long-acting local anesthetic agent around the veins to minimize pain during and after the surgery. The injection forms a cold fluid buffer zone to protect the normal tissue around the varicose veins. At the same time, a large amount of fluid compressing the vein wall towards the heat source increases the effectiveness of cautery of the vein wall from inside.
- EVLT and EVRF are short surgical procedures with low postoperative pain. They can be performed at the operating theatre in the clinic or hospital. They have a low recurrence rate. Patients can walk as usual, immediately after surgery. However, the calf and thigh are better to be elevated above the heart level, for 24 hours after surgery, in order to reduce postoperative swelling, bleeding and bruising. Patients can return to their office work within one to few days. Please consult your doctor for advice.
Small Incision Varicose Vein Surgery: (Hook Extraction / Excision / Cautery / Ligation)
- Small incision varicose vein surgery is a new minimal invasive surgery.
- Experienced surgeons make a tiny incision of 1mm - 5mm over the varicose vein.
- Varicose veins can be treated by hook extraction, excision, cautery, or ligation.
- These procedures can remove medium to small varicose veins and have good cosmetic results.
- As the incisions are small, large numbers of varicose veins can be treated at the same time.
- This procedure can be performed in the clinic or hospital.
- Patients can resume normal walking immediately after the surgery. However, it is better to elevate the calf and thigh above heart level for 24 hours after surgery to reduce postoperative swelling, bleeding, and bruising.
- Patients can return to office work within one to a few days. Please consult your doctor for advice.
Prevention
Patients can relieve varicose vein-associated discomfort and prevent the progression of varicose veins, spider veins, and reticular veins by following these methods:
- Weight control
- Regular exercise to improve leg and vein strength and blood circulation
- Do more leg-raising exercises to promote blood circulation
- Keep your legs flat when sitting
- When resting, lie flat and raise your legs above heart level to promote venous blood return from the lower limbs
- Avoid sitting or standing for long periods of time
- If you have to sit for a long time, do some calf exercises every thirty minutes
- If you have to stand for a long time, shift your weight from one foot to the other every few minutes
- Avoid wearing high-heeled shoes for long periods of time
- Wear compression stockings
- Avoid body-restricting clothing
- Avoid estrogen therapy
FAQs
A: It is very likely. If you suspect yourself suffering from varicose veins, please consult your doctor for advice.
A: Yes. You may choose not to treat varicose veins. But you may feel pain or soreness every time you sit, stand, or walk for an extended period of time. As the condition worsens over time, you may face more serious complications. It is indeed unwise to do so.
For early to moderate disease, if you choose the latest methods to treat varicose veins, you will experience no pain or minor pain during and after treatment. After a few weeks of treating varicose veins, you can return to your favorite activities. Why are you afraid? Why hesitate and not seek treatment early? Please consult your doctor for advice.
A: Varicose veins are associated with the following risk factors: increased venous blood pressure, obesity, prolonged standing and sitting at work, and oral contraceptives. The methods to reduce symptoms of varicose veins are: Control your weight; Avoid wearing tight clothing; Improve blood flow of your lower limbs by taking short breaks several times a day with legs elevated above heart level; Avoid sitting or standing for long periods of time; Change positions frequently to promote blood flow; Avoid oral contraceptive pills; Wear compression stockings. Please consult your doctor for advice.
A: The latest varicose vein surgeries to treat varicose veins are very safe. The surgical procedure is usually short. The postoperative pain is minimal. The recurrence rate is low. Please consult your doctor for advice.