What is hemorrhoid?
Hemorrhoid is the diseased vascular cushion at the anus. Normally, these vascular cushions are situated in the anal canal between the anal skin and the anal sphincter. They are sponge-like vascular structures that help the anal sphincter prevent the leakage of feces or gas through the anal canal. When the anal vascular cushion causes symptoms or complications, it is referred to as hemorrhoid, and treatment for hemorrhoid is required. The aim of treatment is to reduce the symptoms, not to remove all vascular cushions.
Hemorrhoids classifications
Hemorrhoids are classified by their location relative to the dentate (pectinate) line, which is a zigzag line between the anal skin and rectal skin:
- Internal Hemorrhoid: Located above the dentate line.
- External Hemorrhoid: Located below the dentate line.
- Prolapsed Internal Hemorrhoid: Extends both above and below the dentate line.
- Thrombosed External Hemorrhoid: Involves clotted blood inside the blood vessels of the hemorrhoid. It appears as a red-purple firm anal swelling. Patients may experience discomfort or severe rectal pain over this swelling.
Symptoms
- Bleeding during bowel opening/Anal bleeding
- Anal itching/pain
- Mucus discharging from anus with an odor
- Ano-rectal skin prolapse
- Pain during bowel opening
痔瘡可分為四種階段:
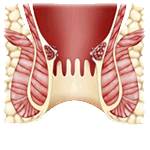
Grade 1:
Bleeding during bowel opening. No prolapsed hemorrhoid.
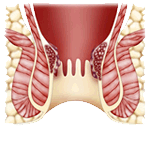
Grade 2:
Bleeding and prolapsed hemorrhoid during bowel opening. Hemorrhoid returns inside the anus spontaneously after bowel opening.
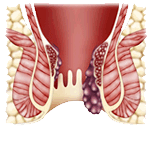
Grade 3:
Hemorrhoid is prolapsed during bowel opening, prolonged standing or carrying heavy objects. It returns inside the anus with the help of finger pushing.
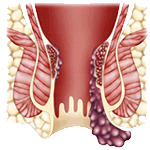
Grade 4:
Hemorrhoid is prolapsed and does not return inside the anal canal.
Severe and Fatal Hemorrhoids
Thrombosis, prolapse, ulceration, or gangrene may occur when complications arise. Specific complications include:
- Gangrene: When gangrene occurs in thrombosed hemorrhoids, infection happens subsequently. Severe degrees of infection can occasionally occur, such as Fournier gangrene. If treatment is not appropriate, such severe infection can lead to bacteremia, septicemia, and rarely, death.
- Severe and persistent bleeding: Severe and persistent hemorrhoidal bleeding may occur, which might cause hemorrhagic shock and death.
Common Sites for Hemorrhoid
As branches of the superior rectal vein are located at the left (3 o’clock), rear right (7 o’clock), and front right (11 o’clock) positions in the anal canal, isolated or a combination of hemorrhoids are mostly found in these positions. These hemorrhoids are called Primary Hemorrhoids.
Hemorrhoids located at the front left (1 o’clock), rear left (5 o’clock), and right (9 o’clock) positions are called Secondary Hemorrhoids.
Most hemorrhoids are Primary Hemorrhoids, located at the 3, 7, and 11 o’clock positions of the anus. Secondary Hemorrhoids are less common. Hemorrhoids can occur at individual positions or any combination of positions.
Hemorrhoid Treatment
Hemorrhoid Treatment Options
Hemorrhoid treatment can be managed through various methods, including:
- Medication:
- Use of oral drugs, anal ointments, suppositories, and stool softeners are the main drug treatments to prevent condition worsening and relieve pain.
- Rubber Band Ligation:
- Suitable for Grade 1 & 2 internal hemorrhoids.
- Suitable for the combination of Grade 1 & 2 internal hemorrhoids with mild external hemorrhoids. After ligation, hemorrhoids will fall off in 7-14 days.
- Transanal Hemorrhoidal Dearterialization:
- Suitable for Grade 1 & 2 internal hemorrhoids.
- Suitable for prolapsed internal hemorrhoids, a combination of Grade 1 & 2 internal hemorrhoids and external hemorrhoids. The surgeon uses an ano-rectal ultrasound scan to locate the hemorrhoidal arteries, then uses sutures to stop the arterial blood flow. After suturing, the blood vessel becomes small and scarred.
- Traditional Hemorrhoidectomy:
- Suitable to cure most hemorrhoid diseases. Due to severe pain after the operation, it is being used less frequently in recent years.
- Stapled Hemorrhoidectomy (SH):
- Surgeons use a circular cutting and stapling tool to cut out the internal hemorrhoids and staple the cut ends at the same time. It is suitable to cure internal hemorrhoids and prolapsed internal hemorrhoids. It causes less pain and allows an early return to work. Additionally, stapled hemorrhoidectomy can lift up the prolapsed anal skin and reposition the external hemorrhoid to the anal canal.
- Harmonic Scalpel (Ultrasound Knife) Hemorrhoidectomy:
- Harmonic scalpel uses ultrasound energy to activate a 2cm long and 1.5mm wide metal rod. The activated metal rod can coagulate tissue protein, cut away the hemorrhoids, and seal off the blood vessels and nerve endings. Harmonic Scalpel Hemorrhoidectomy is suitable for most hemorrhoids. It has a short operating time, very little bleeding, less post-operative pain, less dosage of analgesia, and quick recovery. Patients can return to office work a few days after surgery.
* As the severity of the disease and the general condition of each patient are different, please discuss with your doctor about the best solution for you.
Concerns Before and After Surgery
In Hospital
Preoperative Preparation:
- Start a low residue diet at least 2 days before surgery.
- Eat congee, rice noodles, or macaroni 1 day before surgery.
- Eating is prohibited six hours prior to surgery.
Postoperative Precautions:
- Maintain a low residue diet before complete healing.
- Avoid eating spicy food and drinking alcohol.
- Follow up in the clinic 3-7 days after surgery, then a few weeks afterwards.
In Clinic
Preoperative Preparation:
- Start a low residue diet at least 2 days before surgery.
- Eat congee, rice noodles, or macaroni 1 day before surgery.
- Eating is prohibited six hours prior to surgery.
Postoperative Precautions:
- Maintain a low residue diet before complete healing.
- Avoid eating spicy food and drinking alcohol.
- Follow up in the clinic 3-7 days after surgery, then a few weeks afterwards.
How to prevent hemorrhoid?
To prevent hemorrhoids and maintain overall health, consider the following tips:
- Maintain a good diet habit:
- Drink a minimum of 8 glasses of water a day.
- Eat 2 portions of fruit and 3 portions of vegetables (1 portion = half a bowl) every day.
- Exercise regularly:
- Exercise for 30 minutes every day or have aerobic exercise for 30 minutes, twice a week.
- Avoid prolonged sitting or standing:
- Change your posture frequently.
- Develop healthy bowel habits:
- Develop a daily bowel habit to prevent constipation.
- Avoid excessive force during bowel movements and avoid prolonged sitting on the toilet.
- Dietary precautions:
- Avoid eating spicy food and drinking alcohol.
FAQs
A: Bleeding during bowel opening is a common symptom among digestive tract diseases. Bleeding hemorrhoids are the most common cause of anal bleeding, but it may due to other diseases, e.g. anal fissure, colorectal polyps, dysentery or colon cancer. Please consult your doctor to confirm the diagnosis and arrange necessary investigation or treatment.
A: Pain in bowel movement may be caused by hemorrhoids, abscesses, fistula or anal fissure.
A: The best way to cure and prevent hemorrhoid is to develop a good diet and bowel habit. Sometimes, hemorrhoids recur due to poor diet and bowel habit. Occasionally, the hemorrhoid surgery is futile or if there is some other diseases mimic hemorrhoids. Please consult your doctor to confirm the diagnosis and arrange necessary investigation or treatment if you think your hemorrhoid relapse after surgery.
A: Bowel opening is controlled by anal sphincter. When the anal ring sphincter contracts, it tightens the anus to prevent fecal incontinence. In hemorrhoid surgery, surgeons only remove the redundant skin and subcutaneous hemorrhoid. Surgeons protect the anal sphincter. After hemorrhoid surgery, patient may have pain and difficulty during sphincter tightening to prevent leakage of flatus or feces.
A: As hemorrhoids act as a group of cushions to prevent the leakage of flatus, water and faces, anal sphincter usually do not need to contract vigorously to prevent incontinence. The hemorrhoids surgery cut away the soft tissue, the anal sphincter need more effort to contract. Excessive sphincter contraction after hemorrhoid surgery may cause wound pain. So patients feel difficult to tighten anus because of pain and may have temporary and minimal gas or fecal incontinence. When the wound pain is minimal one week after surgery, fecal incontinence would disappear.
- Maintain a good diet habit
- Drink plenty of water, at least 8 glasses or 2 liters a day
- Eat more fruits and vegetables, eat 2 portions of fruit and 3 portions of vegetables
- Exercise twice a week and 30 minutes each time
- Avoid prolonged sitting or standing. Change the posture frequently
- Develop a daily bowel habit, to prevent constipation
- Avoid excessive force during bowel opening. Avoid prolonged sitting on toilet bowl
- Avoid eating spicy food and alcohol