What is Anal Fissure?
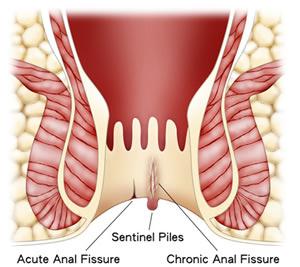
Anal fissure means a skin tear in the anal canal. It is a common anal disease. It mostly happens in the midline posteriorly or anteriorly. Anal fissure can be classified as acute anal fissure, chronic anal fissure, and secondary anal fissure:
- Acute anal fissure: Means the tear in the superficial skin of the anal canal.
- Chronic anal fissure: In chronic anal fissure, the whole skin layer of the anal canal is torn and the underlying sphincter is exposed.
- Secondary anal fissures: Develop due to diseased skin with wounds or poorly healing wounds (e.g., Crohn's disease or after anal surgery (hemorrhoidectomy or fistulotomy)).
Causes
Anal fissure is mainly caused by elevated internal anal sphincter muscle tone and constipation or hard feces. During bowel opening, patients feel pain when hard feces cut the anal skin and cause the fissure. When there is pain, the internal anal sphincter contracts vigorously. The persistent elevated resting level of internal anal sphincter muscle (involuntary) contraction results in less blood flowing to anal tissue and the anal fissure wound. This will result in poor healing or non-healing of the anal fissure.
If there is a tear in the anal skin, our body will attempt to heal the tear. Scar tissue will grow around the fissure, causing the formation of inflammation and connective tissue overgrowth, known as hypertrophic papilla and sentinel pile.
Symptoms
- Anal pain during/after defecation
- Anal itchiness
- Blood in stool / blood dripping down from anus / blood-stained tissue paper after use
- Constipation
- Hard stool
- A few will have diarrhea
Clinical Examination
Anal Inspection
External observation of the anus.
Digital Rectal Examination
Doctors use a gloved finger to palpate the anus and rectum.
Proctoscope / Anoscope Examination
Doctors use a proctoscope / anoscope to have a visual examination of the lower rectum and anal canal.
Surgeons will separate the buttocks around the anus and observe whether there are cracks in the superficial skin in front or behind the anus, whether there are sentinel piles, hypertrophic papilloma, or the internal sphincter muscle fiber in the center of the chronic anal fissure base.
When probing the anus with a finger, surgeons will check if there are hard scars around the anal canal, hard faeces, rectal cancer, and stenosis/tightening of the anus. During the examination, it is necessary to diagnose whether there are haemorrhoids, rectal cancer, anal cancer, or inflammatory bowel diseases, such as Crohn's disease.
Anal Fissure Treatment
Drink 2-3L of water per day. Do some core body exercise to stimulate gut movement. Eat food that can pass through the gut easily. Avoid rough and trunky vegetable fiber. These simple measures can improve constipation. Most simple acute anal fissures (~90%) can be easily controlled/cured with medication and the measures mentioned above.
Medications
The main options for medication include oral stool softeners, anal ointments, and anal suppositories. Anal ointments and suppositories contain local anaesthetic agents, anti-inflammatory drugs, lubricants, anal muscle relaxants, steroids, or haemostatic drugs to quickly relieve the symptoms of anal fissures.
Acute Anal Fissure
Acute Anal Fissure Treatment
- Soaked in warm water bath / sitz bath: Soak in 40°C water to lower the anal sphincter pressure.
- Develop good dietary and bowel habits.
- Oral medication: Stool softener.
- Use anal ointment / suppositories with the following medicines: Local anesthetic, anti-inflammatory, muscle relaxant, lubricant, steroid, or hemostatic agent.
Chronic Anal Fissure
Botulinum toxin is injected into the internal anal sphincter to treat chronic anal fissure. The involuntary contraction of the internal anal sphincter will stop and the blood flow to the chronic anal fissure wound will improve. Chronic anal fissure wounds usually heal within 3 months. The chronic anal fissure healing success rate is over 70-80% within 3 months. If patients with chronic anal fissures do not heal within 3 months, repeated injections of larger doses of botulinum toxin can achieve an overall cure rate of over 80-90% for chronic anal fissures.
If Botox injections fail multiple times or the patient is allergic to the drug, patients may consider surgery for chronic anal fissures.
Surgical Treatment
When chronic anal fissures occur with sentinel piles or hypertrophic papilloma, surgery can be considered. The main principles of surgery are:
- Transverse internal sphincter incision surgery (lateral sphincterotomy): Incision and relaxation of part of the tight internal anal sphincter, reducing intra-anal pressure, allowing the anus to relax, and allowing smooth defecation without incontinence.
- Use electrocautery to stop bleeding from bleeding vessels at the edge of chronic anal fissure ulcers.
- Remove sentinel haemorrhoids and hyperplastic papillomas.
The incision wound of transverse internal sphincter incision surgery and wounds of chronic anal fissures usually heal within 3 to 6 weeks, and the overall healing rate can reach over 90-95%. The involuntary circular contractions of the internal anal sphincter will not be possible, and blood flow to the chronic anal fissure wound will improve. Chronic anal fissure wounds usually heal within 3 months.
Clinical studies have found that transverse internal sphincter relaxing incision surgery is more effective in healing chronic anal fissures than Botulinum Toxin sphincter injection.